Hepatitis C: English
Related Resources
Hepatitis C Illness and Care Journey (HCV ICJ)
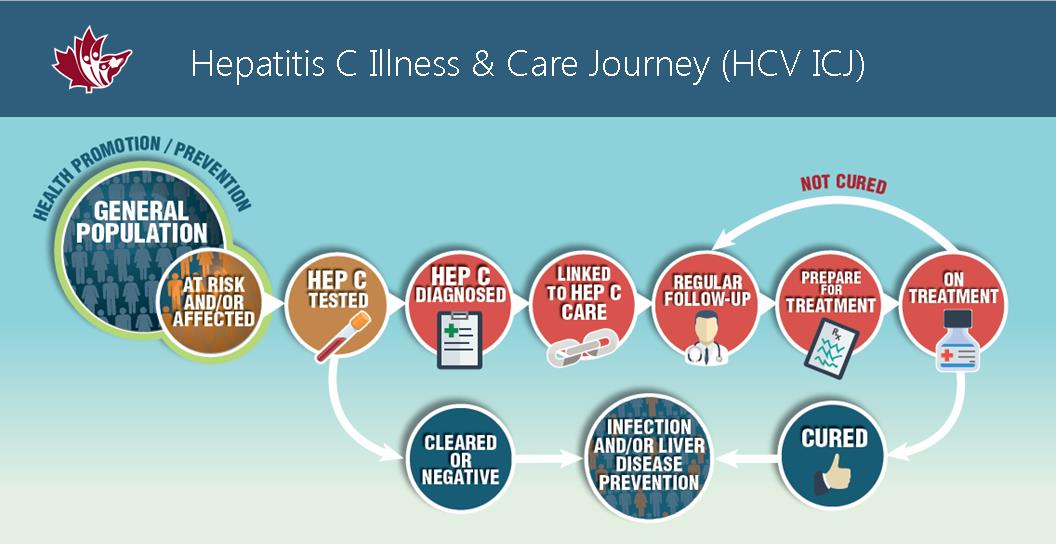 See resources that go with each stage of the HCV ICJ.
See resources that go with each stage of the HCV ICJ.
Video: Frequently asked questions about hepatitis C (Booklet Version)
 Answers questions most often asked by people with hepatitis C (5 minutes).
Answers questions most often asked by people with hepatitis C (5 minutes).
Basic facts about hepatitis C
(video transcript)
What is hepatitis C?
It’s a virus that can cause damage to the liver, an organ that has many different functions essential to your life.
How many people in Canada have it?
About 300,000 people in Canada have hepatitis C. That is about 1 in every 100 people.
Can the body get rid of the infection?
Sometimes, yes. For every 10 people that get hepatitis C, about three will be able to get rid of the infection in the first six months. Their body attacks the virus and gets rid of it naturally. About 7 will have chronic hepatitis C. That is, they will likely have it for life, unless they get treatment.
Can hepatitis C be cured?
Yes! New medications can cure over 95% of those treated.
Is there a vaccine for hepatitis C?
No, there is no vaccine to protect you from getting hepatitis C. You can protect yourself by knowing how it is spread and taking actions to reduce the risks of getting hepatitis C.
If I get hepatitis C, will I know I have it?
Unless you are aware of the activities that put you at risk of getting hepatitis C, you will probably not know you have it. This is because most people do not have symptoms right away.
Only about 1 in 4 people have symptoms when first infected. Many people do not have symptoms for 10 to 30 years after being infected. This is because the liver can keep doing its job for a long time, even when it is damaged.
What are the symptoms of hepatitis C?
Early on, most people will have no or few symptoms, but over time, some may experience:
- feeling tired
- muscle or joint pain
- headaches
- itchy skin
- depression
- anxiety
- abdominal pain in and around the liver
- brain fog (having a hard time concentrating and suffering from memory lapses)
Sorting out the symptoms
Many people with hepatitis C are living with more than one condition. This can make it difficult to sort out which symptoms are related to hepatitis C. See your health care provider if you are having symptoms that you are concerned about.
How hepatitis C is spread?
(video transcript)
Importance of understanding how hepatitis C is spread
After learning about hepatitis C, some wonder if people they know have it. But, you cannot tell from looking at a person if they have hepatitis C.
This is why it is important to know how hepatitis C is spread and how it is not spread. Then you can take actions to try to protect yourself or others from getting hepatitis C.
Hepatitis C is not spread through…
coughing, hugging, kissing; sharing dishes, drinking water, or clothes; swimming pools or toilets. These day-to-day activities, and others like them, are safe.
Hepatitis C is passed through blood-to-blood contact.
How to prevent the spread of hepatitis C
First, know how blood-to-blood contact can happen. You can get hepatitis C if the blood of a person who has the virus gets into your blood. Some activities are more likely to lead to blood-to-blood contact than others. The greater the chance of blood-to-blood contact, the greater the chance that hepatitis C will be spread.
Blood and blood products
The most effective way for hepatitis C to get into your body is directly into your bloodstream.
In the past, before 1992, there was a fairly big risk of getting hepatitis C through blood transfusions. This was before donated blood was tested for the presence of the hepatitis C virus.
In Canada, since 1992*, all donated blood is tested for hepatitis C so there is no longer a big risk of catching it from blood transfusions.
*Testing began in 1990, but a more sensitive test was used starting in 1992.
Today, hepatitis C is most often caught…
…when people share drugs or injection drug equipment. If the drugs or injection equipment is used for more than one person, it is quite possible for hepatitis C to spread from someone who has the disease to another person.
This is why injecting supplies (like syringes, water, spoons/cookers and cotton) are sometimes supplied free of charge to people who inject drugs. Otherwise, if people share injection equipment they are at higher risk of getting hepatitis C.
Because it is so easy for hepatitis C to get into the bloodstream through any kind of injection, all medical procedures must be done using new disposable syringes and sterilized equipment.
Hepatitis C can sometimes be caught…
…when the blood of an infected person comes into contact with another person’s body through something like an open sore, a cut or a piercing. For example, hepatitis C can get into the body through:
- the use of unsterile or reused equipment during tattooing, cutting, and body piercings
- from risky sexual practices that lead to the exchange of blood, like in rough sex
- or by sharing non-injection drug equipment, like straws or crack pipes
Unprotected sex and hepatitis C…
Hepatitis C can be passed through unprotected sex if blood is present.
Examples include sex between:
- men and women,
- men and men, or
- during sexual assault (both the victim and offender are at risk)
Also, the risk of passing hepatitis C through sex is higher when there is a co-infection with HIV, hepatitis B or other sexually passed infections. This is because other infections can cause sores or cuts that might bleed.
To protect yourself…
Use a condom if you think there might be rough sex or when HIV or other sexually transmitted infections (STIs) might be present.
If you have been sexually assaulted, see a health care provider for testing and other supports.
It is also possible for hepatitis C to be caught…
- from sharing household articles that could have blood on them like razors, toothbrushes or nail clippers
- by accidentally being poked with a used needle, or
- from medical or dental procedures if the equipment is reused and has not been properly sterilized
Although it doesn’t happen very often, it is possible for hepatitis C to spread from a mother to her baby at birth.
Related Resources
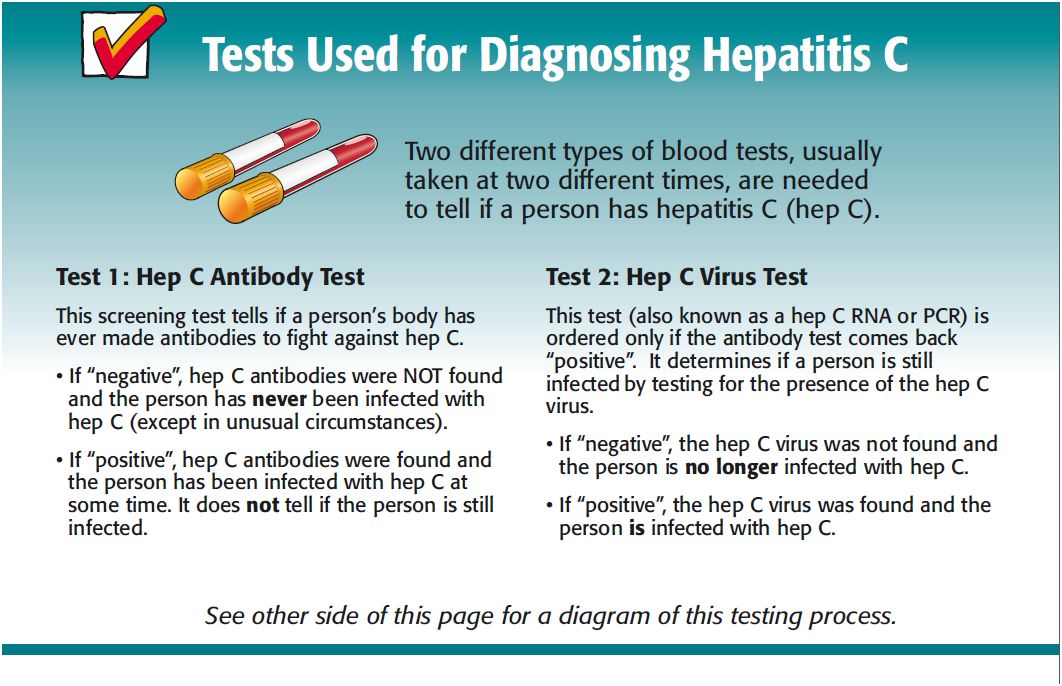
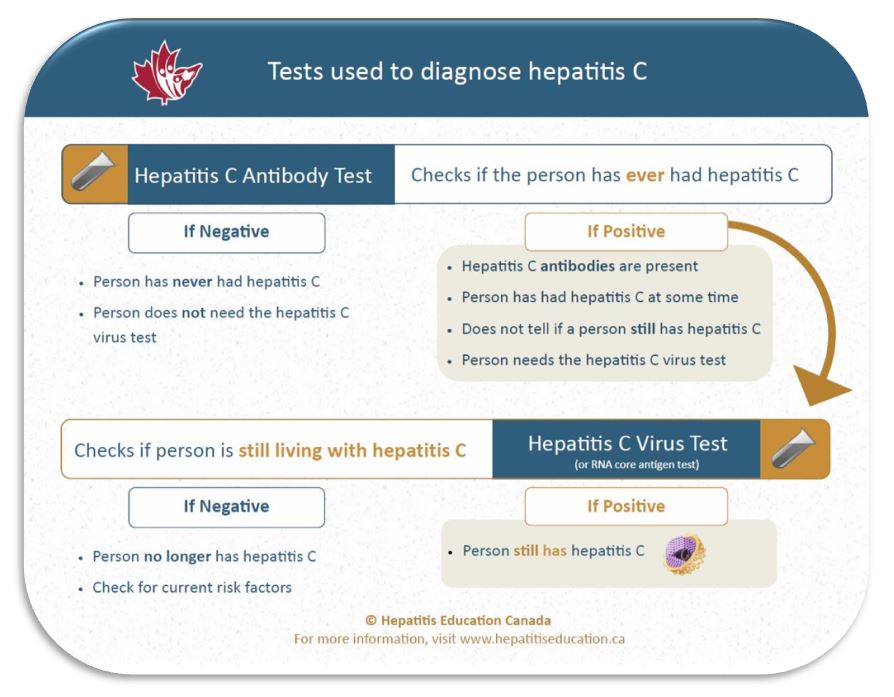
Patient Page: Tests used for diagnosing hepatitis C
This patient page explains the hepatitis C testing process (with diagram).
Provider Page: Hepatitis C Virus Pre- and Post-test checklists
 Discussion checklists for providers to use with patients before/after the antibody and RNA tests.
Discussion checklists for providers to use with patients before/after the antibody and RNA tests.
Getting tested for hepatitis C
(video transcript)
Should I get tested to see if I have it?
You should get tested if you have had even one risk event, a long time ago or recently. Getting your blood tested is the only way to know for sure if you have or do not have hepatitis C.
How do I get tested?
You can go to any health care provider, like a nurse or doctor, to ask about how and where to get tested for hepatitis C.
How many types of blood tests are done to diagnose a current hepatitis C infection?
Often, two types of blood tests are often done to diagnose a current hepatitis C infection. These tests are usually done at two different times.
What is the first test?
The first test you will get is the hepatitis C antibody test. This test shows if you have ever been infected with hepatitis C. It does not tell if you are still infected.
What if the first test is “negative”?
If the first test, the antibody test, is negative, it means that hepatitis C antibodies were not found and you have never been infected with hepatitis C. You do not need to get the second blood test.
What if the first test is positive?
If the antibody test is positive, hepatitis C antibodies were found and you have been infected with hepatitis C at some time. This test does not tell if you are still infected so you will need the second test.
What does the second test check?
The next test is the hepatitis C virus test (also known as hepatitis C RNA or PCR). This second test checks to see if you are still infected with hepatitis C.
What if the second test is negative?
If the hepatitis C virus test is negative, the hepatitis C virus was not found so you are no longer infected with hepatitis C.
But, since it is possible to catch hepatitis C more than once, you may want to talk to a health care provider about how to prevent getting hepatitis C again.
What if the second test is positive?
If the hepatitis C virus test is positive, the hepatitis C virus was found. This means you have hepatitis C.
Your test result must be sent to your local public health department so they can count how many people have hepatitis C.
However, your hepatitis C diagnosis is kept confidential. You are not required to tell anyone that you have hepatitis C. You can choose who to tell.
Related Resources
Patient Page: Questions people frequently ask their providers about hepatitis C
 A checklist of questions people frequently ask their health care providers about hepatitis C.
A checklist of questions people frequently ask their health care providers about hepatitis C.
Patient Page: Personal bill of rights
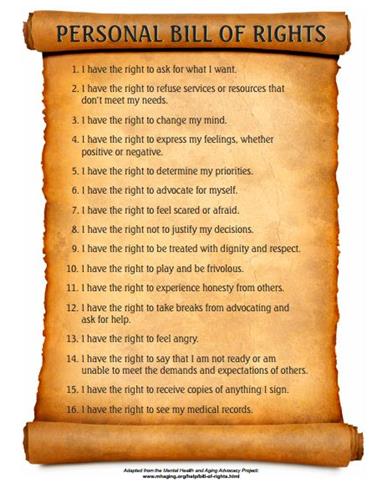 This personal bill of rights may help you to speak up for yourself.
This personal bill of rights may help you to speak up for yourself.
If I have hepatitis C, what should I know and what’s next?
(video transcript)
What hepatitis C can do to the body
Hepatitis C can cause swelling and scarring in the liver. After 20 to 30 years, the liver can become quite damaged and unable to work properly. This can cause many different health problems because the liver does so many important jobs for the body.
Anyone with signs of liver damage should be checked to see if they can get hepatitis C treatment as it could stop further liver damage.
How can I know if my liver is damaged
Health care providers cannot predict who will have liver damage, so it is important to regularly see a provider who can monitor your health.
Your health care provider can complete a detailed health assessment. This assessment will help to find out if the hepatitis C infection has caused any problems in how well your liver works. It may include:
- a physical examination
- blood tests, and
- other tests, like a liver ultrasound
What is a hepatitis C viral load (HCV RNA) test?
A Hepatitis C RNA test checks your blood for the presence of the hepatitis C virus.
Some RNA tests check if the hepatitis C virus is in the blood, but not how much virus in the blood. These tests tell if you still have hepatitis C.
Other RNA tests check how much hepatitis C virus is in the blood. If you are being treated for hepatitis C, these tests will tell if treatment is working.
Questions to ask your health care provider
It is important to ask your provider for more information about:
- hepatitis C
- treatment for hepatitis C
- deciding who to tell that you have hepatitis C
- how you can stay healthy, and about
- vaccinations such as hepatitis A, B, pneumonia, and influenza
These vaccinations are free for people living with Hepatitis C. You can get these vaccinations from your health care provider or public health unit.
About sources of information
There are many sources of hepatitis C information such as the internet, friends & family, and health care providers. Information can sometimes be out of date or incorrect.
It is important to check out the information and decide if the information is helpful in your situation.
When to see a specialist/or go to a liver clinic
This will vary, but most people get a referral when thinking about going for treatment. You may need a referral from your health care provider to see a hepatitis C specialist or to go to a liver clinic.
Do people living with hepatitis C need to see a health care provider even if they feel fine?
Yes. They should see their provider every 6 to 12 months. Even if a person feels well and has no symptoms, hepatitis C can still be damaging their liver.
How often to see a health care provider
See a provider every 6 months if your last checkup showed you did have liver damage.
See a provider every 12 months if your last checkup showed you did not have liver damage.
In addition to these regular check-ups, see a provider anytime you have questions or concerns.
Deciding who to tell
Sometimes people newly diagnosed with an infectious disease are reluctant to talk about it. They are not sure how others will react.
For example, many people don’t know much about hepatitis C, so those infected worry that friends or family will become overly cautious or afraid of catching it.
Before telling others that you have hepatitis C, take your time to think about it. There is no rush, but it is important to have some friends or family know so that you can have their support. When deciding who to tell, ask yourself:
- who will understand
- who can I trust to respect my privacy and feelings, and
- who can give me emotional support</>
Understanding stigma
Stigma happens when somebody is judged or not valued as a person. People with hepatitis C sometimes feel judged or not valued because they have hepatitis C.
Stigma can happen for many reasons; one reason can be fear that comes from a lack of knowledge. People may be afraid because they don’t know about how hepatitis C is spread from person to person, how it affects health or how it is treated.
Getting the healthcare you need
It’s important to get the health care you need but it can be hard to ask for it.
This “Personal Bill of Rights” is one support that might help you to speak up for yourself.
Related Resources
Patient Book: Speaking up for care and support
 A skills building workbook to help people get the care and support they need (25 pages).
A skills building workbook to help people get the care and support they need (25 pages).
Patient Card: Tips to getting your message heard
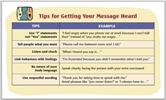 6 tips on how to get people to hear you and what to do when people say “no.”
6 tips on how to get people to hear you and what to do when people say “no.”
Healthy balance
(video transcript)
Finding a healthy balance
Learning to balance a chronic disease like hepatitis C with other things going on in your life can take time. You may have to juggle several different priorities all at once.
Deciding what to do first and how much time to spend on each thing will depend on your situation.
Staying healthy
To help keep your physical and emotional life balanced, try to:
- stay connected. Having a chronic infectious disease can affect your social life and leave you feeling isolated.
- figure out who you feel comfortable talking with. It is helpful to have someone who you can talk to about what you are going through and the decisions you need to make.
- reduce physical and emotional stress with exercise and eating a balanced diet.
Do I need a special diet?
Most people with hepatitis C do not need a special diet, but a healthy diet with plenty of vegetables and fruits, whole grains, meat and meat alternatives (e.g., tofu) can improve overall health and help the liver to work better.
There is evidence that regularly drinking caffeinated coffee may slow the progression of liver disease (Kennedy et. al. 2016; evidence is clearer for caffeinated coffee than for decaffeinated), but talk with your provider as it may have negative impacts on other areas of health.
You may need a special diet if you are on hepatitis C treatment or if you have liver damage or other health concerns such as:
- HIV,
- alcohol dependency,
- kidney disease,
- diabetes, or
- are overweight (from 2003 Dieticians of Canada HEP guidelines)
In these cases, speak to your health care provider or nutritionist to learn about what you need to eat and what to avoid.
Do I need to avoid alcohol, drugs or certain medications?
It depends. Your liver removes toxins from your bloodstream. This can be things like alcohol, supplements, medications or other drugs. When there are too many toxins to remove, your liver can get damaged. Talk with your provider about your situation.
Alcohol
Drinking alcohol can cause liver damage. Liver damage from alcohol can happen quicker for people who have hepatitis C. Talk to your provider about alcohol use, how it can affect the liver and the treatment of hepatitis C, and if you need to cut down on alcohol use.
Supplements
Tell your health care provider everything you are taking. Some people use herbal remedies or other supplements along with over-the-counter drugs.
Some medicines, supplements or natural remedies can be harmful for your liver when taken alone or with medicine prescribed by your provider.
Examples of what can be harmful…
Some examples of what can be harmful to your liver include:
- too much acetaminophen (watch for it in multi-drug medications, such as cold and flu medicines)
- non-steroidal anti-inflammatories (if you have cirrhosis)
- iron
- licorice root
- St. John’s Wort
Tell your health care provider everything you are taking to find out what is safe for you.
Related Resources
Treatment
What are the treatments for hepatitis C?
Current treatments are very different from old therapies that included interferon.
They:
- Usually take 8 to 12 weeks
- Involve only oral treatments, such as pills or tablets instead of injections, and
- have much fewer and less severe side effects
- And have cure rates higher than 95%
NEW!: Treatment is now available across Canada. Ask your health care provider about getting treatment in your province/territory
Can I get treatment if I have other health issues?
Yes. Talk with a health care provider. You may need to be referred to a provider who has experience treating hepatitis C for people who have other health challenges.
Some providers have experience treating hepatitis C for people who also live with:
- HIV,
- diabetes,
- mental health challenges, or
- addictions (e.g., alcohol, injection drugs, methadone)
How do I get treatment?
Speak to your health care provider about getting HCV treatment.
If I get cured, will I have hepatitis C antibodies?
Yes! Getting cured of the hepatitis C virus does not get rid of the hepatitis C antibodies in your blood. These are made by your immune system to try to fight the virus. Once you are cured, the blood test for the:
- the hepatitis C antibody will still be “positive”, but
- the test for the hepatitis C virus will be “negative”
Being cured does not protect you…
It is important to remember, that being cured does not protect you from getting hepatitis C again.
Only protecting yourself from contact with blood will protect you from getting a new hepatitis C infection.
Protecting yourself from contact with blood will also decrease the chance of getting other blood-borne infections. But, keep in mind that some infections, like HIV and hepatitis B, are passed through blood AND other body fluids.
Getting ready for life after treatment
People often make many changes before and during treatment. For example, they might gain support networks of friends and health care providers, or make changes to diet and physical activity. But what will happen after treatment ends?
Talk with your team about life after treatment
Here are some things for you and your care team to talk about:
- Will my care team change?
- Will I need to change my supports?
- If I am cured, will I feel better right away?