Reasons why some people do not go for hepatitis C care
The HCV Illness & Care Journey (HCV ICJ)
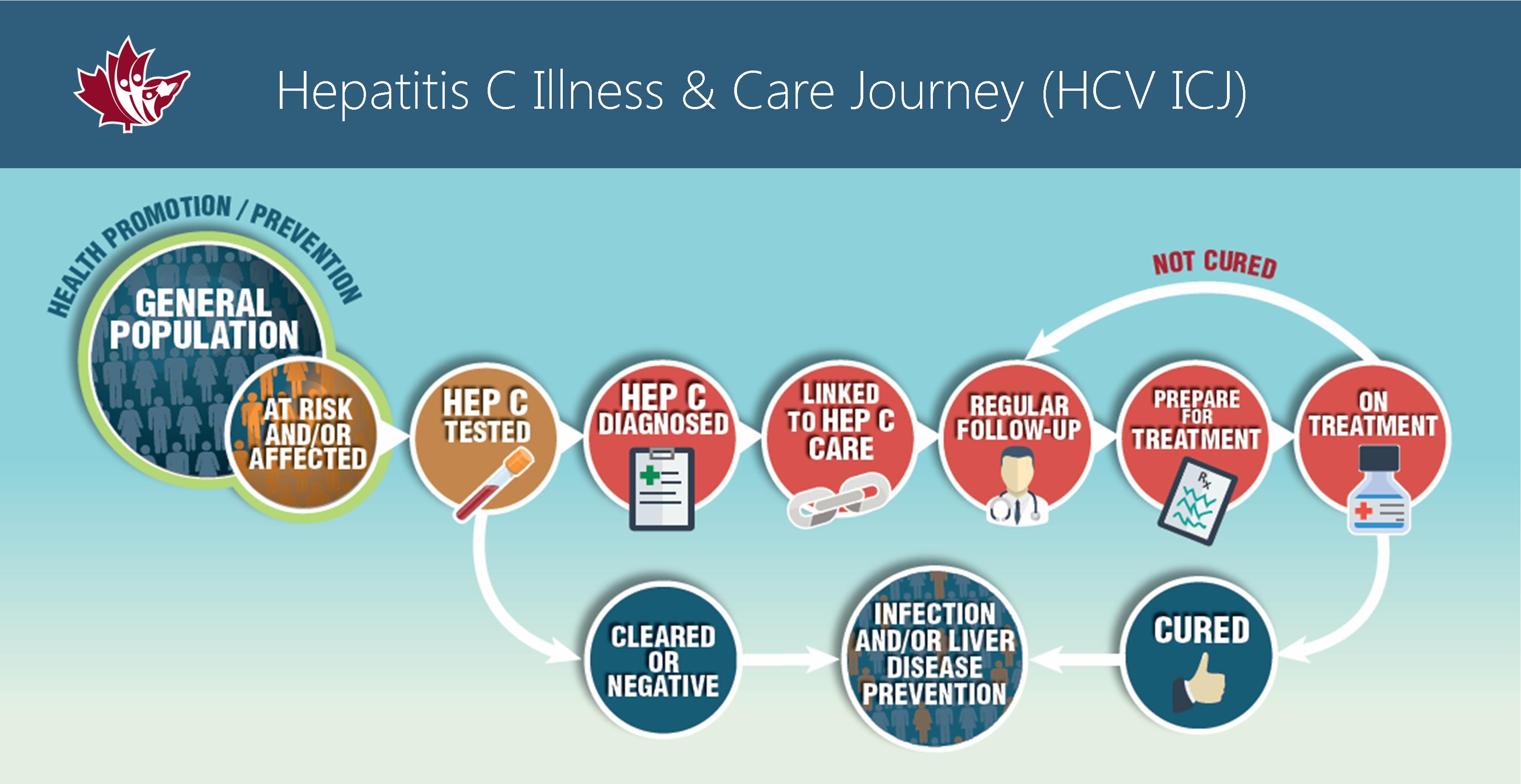 View the HCV ICJ: key journey points for people at-risk or diagnosed with hepatitis C and resources that go with each stage of care.
View the HCV ICJ: key journey points for people at-risk or diagnosed with hepatitis C and resources that go with each stage of care.
Why some do not go for hepatitis C care:
1. Self- protection
(video transcript)
The first theme is called self protection because we discovered that participants put off or avoided coming for health care to protect themselves.
For example, frequently participants told us that when they were diagnosed or when they disclosed that they had hepatitis C they were treated differently- and not in a good way- they often spoke of rude and judgmental treatment.
Some even said that they put off being tested for hepatitis C because of the way they had seen others treated.
Others spoke of not wanting to go to a hepatitis C specialist clinic in case someone in the waiting room recognized them and would tell others they have hepatitis C.
A number of people gave examples of why they avoided emergency departments even at great personal expense. They spoke of Poor treatment such as, being accused of drug seeking, being ignored for long periods of time, or not being adequately assessed.
Many spoke of the wanting to keep their diagnosis a secret to protect themselves from stigma and discrimination and how difficult that is especially in rural and remote areas.
Reasons some do not go for hepatitis C care:
2. Not understanding the benefits
(video transcript)
There were several reasons why participants had difficulty seeing the benefit of attendance.
The first bullet is highlighted because we were surprised to find that many participants did not receive advice from their medical care provider about how often they should return to have a hepatitis C reassessment – and most found out about treatment on their own- not through providers.
This lack of advice for follow-up or treatment accounted for lapses in attendance for hepatitis C care that could span several years
Others pointed out that their family doctor didn’t seem to know as much about hepatitis as they did so they didn’t benefit from attendance.
Others spoke of weighing the costs versus the benefits of going to the doctor or going on hepatitis C treatment when they didn’t have troublesome symptoms: “the point of treating something that’s not bothering me at this point in time and make myself sick for the next six months, well, it doesn’t make a lot of sense to me.”
Reasons some do not go for hepatitis C care:
3. Competing priorities
(video transcript)
Many spoke of the competing priorities in their life which resulted in them putting hepatitis C into the background of their lives.
Some said that other priorities like earning a living or caring for family members took all their time.
While others talked about periods of instability in their lives that kept them from accessing care because they had to manage other priorities like finding shelter, or food or money.
As I mentioned earlier several participants had more than one condition they had to manage so that took their time and attention: “…….. I got so much things wrong with me I, just like, oh, like it’s my arthritis or whatever, like, I completely forgot I had hep C.”
Still others spoke of being so sick from hepatitis C that they didn’t have the energy to attend all their appointments or they spoke of having brain fog from their illness and missing some of their appointments because they forgot about them.
Reasons some do not go for hepatitis C care:
4. Knowledge gaps
(video transcript)
On this slide I will highlight a few of the issues for the theme we call knowledge gaps and health literacy.
Participants pointed out that both providers and those affected needed to gain more knowledge about hepatitis C and to have more information available especially about what tests should be done to monitor for progression of hepatitis C disease such as liver fibrosis or cirrhosis and how often the tests should be done.
Participants said that most of the misinformation they received came from primary care providers – the participants thought these providers have to deal with lots of diseases and may not have had much hepatitis C education in their training programs.
The second bullet is a quote from a provider who participated in the study who said: “On the helpline, I receive calls from people from all over… and the first information they receive is from a doctor who … says that it cannot be treated.”
The other thing that goes hand in hand with getting information is the ability to understand the information – or Health Literacy.
Participants spoke of the difficulty understanding medical terms and feeling uncomfortable asking about what the terms meant especially when they had a limited amount of time with the physician.
The other issue was how to sort through information from multiple sources and how to decide what or who to believe
Reasons some do not go for hepatitis C care:
5. Access to services
(video transcript)
As mentioned earlier, these final two themes focus on the fact that the way health services are organized and delivered can affect a person’s ability to attend for care.
An important issue is the out of pocket costs for people on limited budgets – the costs of parking or travel to specialist clinics can add up over time and be prohibitive.
In some areas especially rural and remote areas- there are shortages of family physicians and specialists or social support services are not available.
Accompanying physician shortages are long wait times for appointments which participants said was very discouraging and often led to non-attendance.
Participants described in great detail the plans and preparations they made while they were waiting to see a specialist and get started on the 6 to 12 month course of anti-viral therapy.
Unfortunately, participants did not know that there could be a lengthy pretreatment period in which they would have to undergo more tests or have consultations by other specialists to make sure that it was safe for them to take the anti-viral therapy- delays in starting therapy although necessary could also result in decisions to drop out or defer treatment.
Sometimes people didn’t have access to care because they had been refused services for missing appointments or if they admitted to using illicit drugs.
Participants pointed out that the lack of integrated or culturally appropriate services acted as a barrier to care. For example, many spoke of how helpful it was to work with nurses who could help them manage their symptoms or get through a difficult treatment regime and how important it was to have social support workers who could assist them with personal issues and accessing resources.
Reasons some do not go for hepatitis C care:
6. Restrictive policies
(video transcript)
In this final theme I will highlight some of the policies that discourage attendance for health care services.
Even though the eligibility criteria have changed, the study participants pointed out a general belief that it is necessary to abstain from illicit drugs for at least 6 months before attempting to access treatment with anti-viral therapy.
Participants also described that treatment eligibility criteria varied depending on the province and so depending on where a person lived they may encounter more barriers to accessing treatment.
And finally, some providers or agencies have policies which may make it difficult for some to access their services.
For example the need to make or confirm appointments if you don’t have ready access to a phone, the difficulty getting a referral to a specialist when you don’t have a family doctor, or providers that have penalties such as missing three appointments and you can’t come back.